Fact sheets: Better Care. Smarter Spending. Healthier People:Paying Providers for V alue, Not Volume
- Date
- 2015-01-26
- Title
- Better Care. Smarter Spending. Healthier People:?Paying Providers for V alue, Not Volume
- For Immediate Release by CMS
- Monday, January 26, 2015
- Contact
- press@cms.hhs.gov
Better Care. Smarter Spending. Healthier People: Paying Providers for Value, Not Volume
Rewarding Volume: Where We Are Now
Improving the quality and affordability of care for all Americans has always been a pillar of the Affordable Care Act, alongside expanding access to such care. The law gives us the opportunity to shape the way health care is delivered to patients and to improve the quality of care system-wide while helping to reduce the growth of health care costs.
When it comes to improving the way providers are paid, we want to reward value and care coordination ? rather than volume and care duplication. In partnership with the private sector, the Department of Health and Human Services (HHS) is testing and expanding new health care payment models that can improve health care quality and reduce its cost.
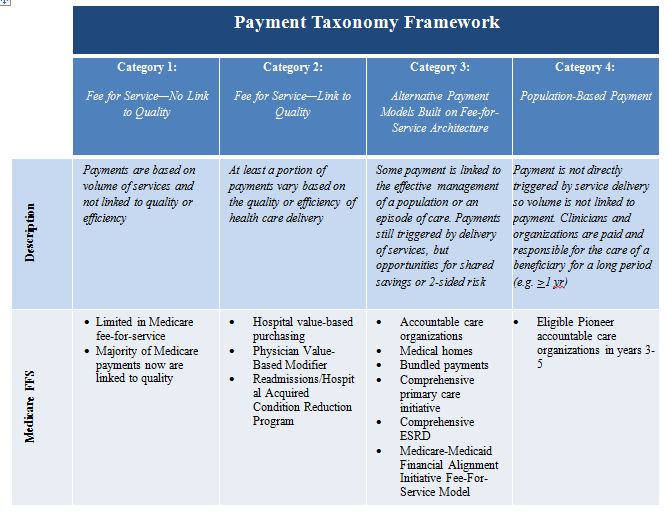
HHS has adopted a framework that categorizes health care payment according to how providers receive payment to provide care.1
- category 1?fee-for-service with no link of payment to quality
- category 2?fee-for-service with a link of payment to quality
- category 3?alternative payment models built on fee-for-service architecture
- category 4?population-based payment
*for more detail and examples, see gPayment Taxonomy Frameworkh
Value-based purchasing includes payments made in categories 2 through 4. Moving from category 1 to category 4 involves two shifts: (1) increasing accountability for both quality and total cost of care and (2) a greater focus on population health management as opposed to payment for specific services.
Prior to 2011, many Medicare payments to providers were tied only to volume, rewarding providers based on how many tests they ran, how many patients they saw, or how many procedures they did, for example, regardless of whether these services helped (or harmed) the patient. But thanks to reforms under the Affordable Care Act and other changes, by 2014, an estimated 20 percent of Medicare reimbursements had shifted to categories 3 and 4, directly linking provider reimbursement to the health and well-being of their patients.
Rewarding Value: Where We Are Going
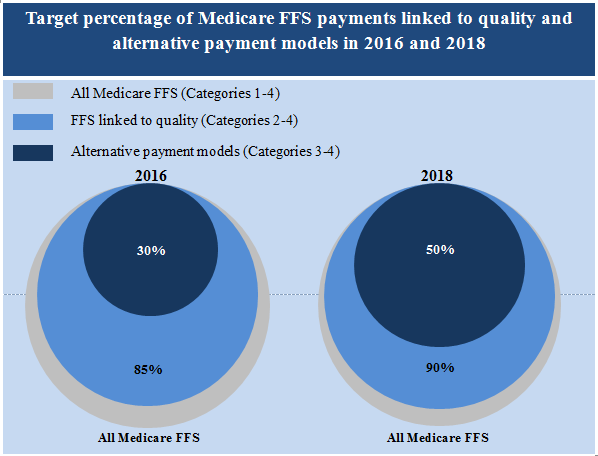
To help drive the health care system towards greater value-based purchasing ? rather than continuing to reward volume regardless of quality of care delivered ? HHS has set a goal to have 30 percent of Medicare payments in alternative payment models (categories 3 and 4) by the end of 2016 and 50 percent in categories 3 and 4 by the end of 2018. This will be achieved through investment in alternative payment models such as Accountable Care Organizations (ACOs), advanced primary care medical home models, new models of bundling payments for episodes of care, and integrated care demonstrations for beneficiaries that are Medicare-Medicaid enrollees. Overall, HHS seeks to have 85 percent of Medicare fee-for-service payments in value-based purchasing categories 2 through 4 by 2016 and 90 percent by 2018.
Three years ago, Medicare had limited payments in alternative payment models, but at the end of 2014 these value-based payments represented approximately 20 percent of Medicare fee-for-service payments to providers. This increase was driven by the Medicare Shared Savings Program (MSSP) and Pioneer ACOs, the Bundled Payment for Care Improvement Initiative, and the Comprehensive Primary Care Initiative, among other programs. HHS is working with private payers, including health plans in the Health Insurance Marketplace and Medicare Advantage plans, as well as state Medicaid programs to move in the same direction toward alternative payment models and value-based payment to providers and to meet or exceed the goals outlined above wherever possible.
How We Get There: Health Care Payment Learning and Action Network
At HHS, we have a responsibility to help align the way providers are paid as a key step toward better care, smarter spending, and healthier people. We also know that we cannot do it alone. Working in concert with our partners in the private, public and non-profit sectors, we are announcing the establishment of the Health Care Payment Learning and Action Network to help align the important work being done across sectors.
All alternative payment models and payment reforms that seek to deliver better care at lower cost share a common pathway for success: providers must make fundamental changes in their day-to-day operations that improve the quality and reduce the cost of health care. Making operational changes will be attractive only if the new alternative payment models and payment reforms are broadly adopted by a critical mass of payers. When providers encounter new payment strategies for one payer, but not others, the incentives to fundamentally change are weak. In fact, a provider that alters its system to prevent admissions and succeed in an alternative payment environment may lose revenue from payers that continue fee-for-service payments.
The Learning and Action Network will accelerate the transition to more advanced payment models by fostering collaboration between HHS, private payers, large employers, providers, consumers, and state and federal partners. Working together, Learning and Action Network partners will:
- Serve as a convening body to facilitate joint implementation and expansion of new models of payment and care delivery
- Identify areas of agreement around movement toward alternative payment models and define how best to report on these new payment models
- Collaborate to generate evidence, share approaches, and remove barriers
- Develop common approaches to core issues such as beneficiary attribution, financial models, benchmarking, and risk adjustment
- Create implementation guides for payers and purchasers
Alignment between HHS, private sector payers, employers, providers, and consumers will help health care payments transition more quickly from pure fee-for-service to alternative payment models ? a critical step toward better care, smarter spending, and healthier people.
1Rajkumar R, Conway PH, Tavenner M. CMS--engaging multiple payers in payment reform. JAMA. 2014 May 21;311(19):1967-8.
###